
Adam R. Guttentag, M.D.
Albert Einstein Medical Center
Philadelphia, Pa
ThoracicFungal Disease


Fungal Infections
•200,000 species of fungi
<200 known to cause human disease
•Mycosis-invasion of tissue by fungi
Superficial mycosis
Cutaneous mycosis
Subcutaneous mycosis
Systemic mycosis
»Primary (immune competent)
»Opportunistic (immune compromised)

Pulmonary Fungal InfectionsClinical presentations
•Asymptomatic
•Acute
•Chronic / Progressive
•Disseminated

Acute Fungal Infection(Competent Host)
•Infested soil disturbed, organisms inhaled
cavers, demolition workers, farmers
•Acute bronchopneumonia (consolidation)
•Enters lymphatics hilar LN’s bloodstream
•Cell-mediated immune response and delayedhypersensitivity (several weeks)
Necrotizing (caseating) granuloma formation
Similar process in LN’s

Acute Fungal Infection(Competent Host)
•Self-limited disease
•May heal completely
•May leave nodule(s) 5 mm. toseveral cm., which can calcify
Latent infection
Partial immunity to reinfection

Chronic / ProgressiveFungal Infection
•Inadequate (or excessive?) hostresponse
•Necrotizing and fibrosinggranulomatous inflammation.
•Some forms indistinguishable frompostprimary TB

Disseminated Infection(Compromised Host)
•May be seen in any fungal infection
•Hematogenous spread early or late incourse of infection
•Miliary nodules 1-4 mm in size
•Systemic involvement liver, spleen,marrow, skin, brain, bone, etc.

Invasive Infection(Compromised Host)
•Aspergillus, zygomycetes e.g. Mucor
•Invasion through bronchial wall intoadjacent artery
•Thrombosis and infarction

Immune Competent Host:Endemic Fungi
•Histoplasma capsulatum
•Coccidioides immitis
•Blastomyces dermatiditis
•(Cryptococcus neoformans)

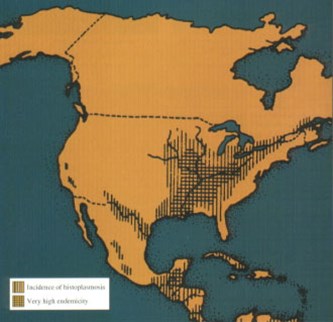
Histoplasmosis
•Endemic in Ohio,Mississippi/ Missouri,andSt. Lawrence river valleys
•Spores in soil rich in batand bird droppings
•Over 80% seropositive inendemic areas

Acute Histoplasmosis
•Estimated 250,000 new cases in US/year
•Most infections asymptomatic or subclinical (>90%)
•Often mild respiratory or flu-like illness
3-14 days after exposure
Fever, cough, chest pain
•Sx depend on:
Inoculum inhaled
Immune status, age, previous exposure
•Sx resolve in weeks to months without treatment

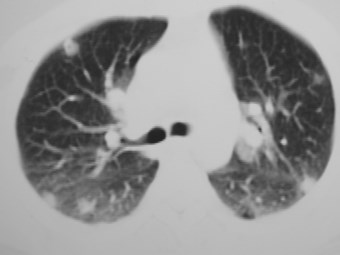
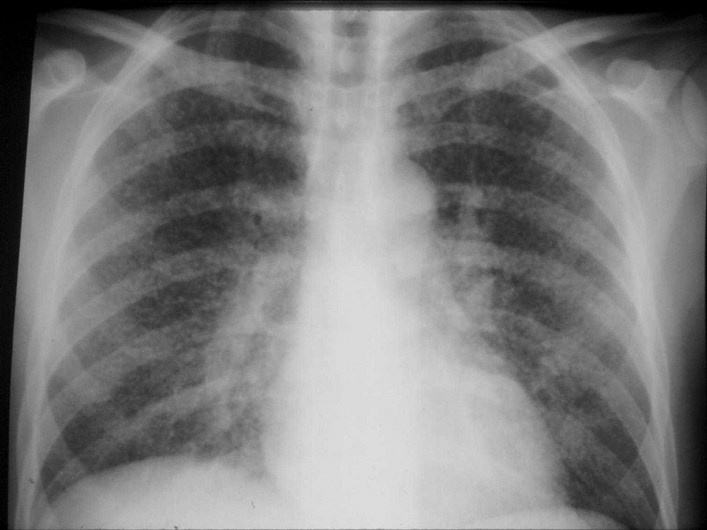
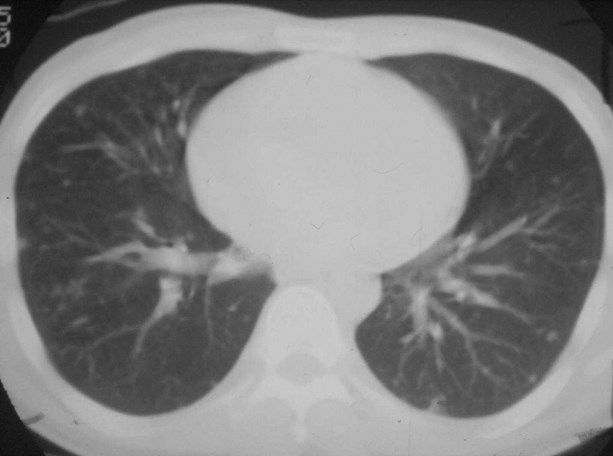
Acute HistoplasmosisRadiology
•Often no X-rays
•Focal consolidation
•Multiple nodular opacities
May cavitate and often calcify
•Adenopathy 5-10%
Rarely isolated adenopathy
»Esp. in children (like TB)


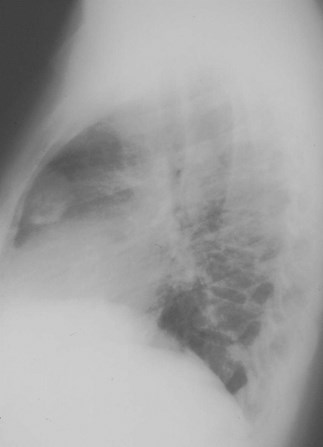
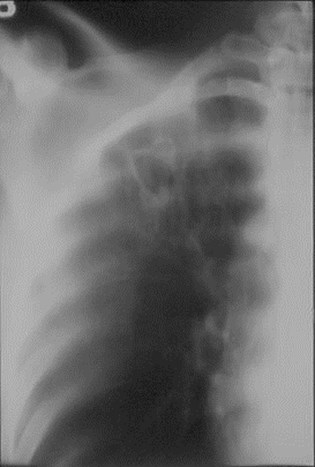
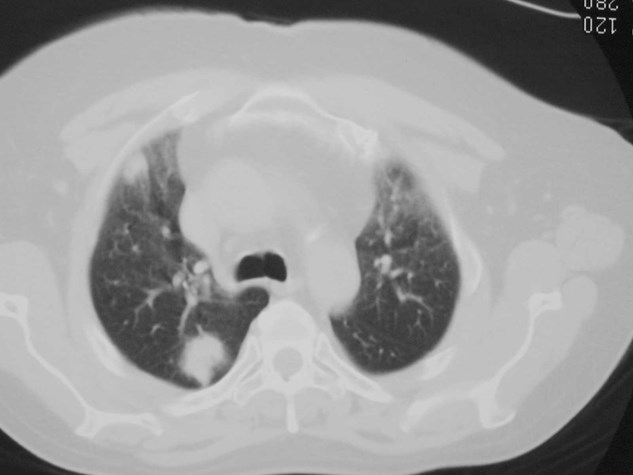
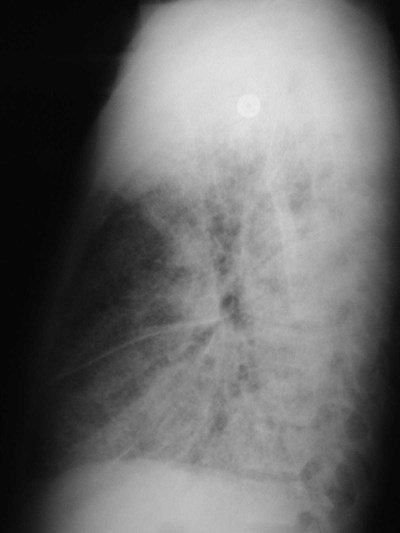
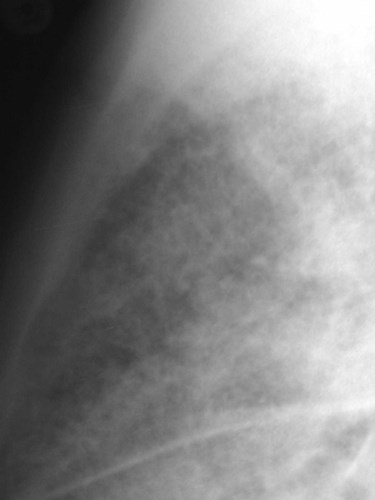
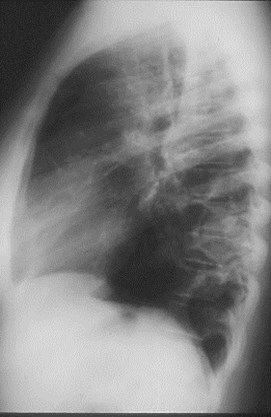
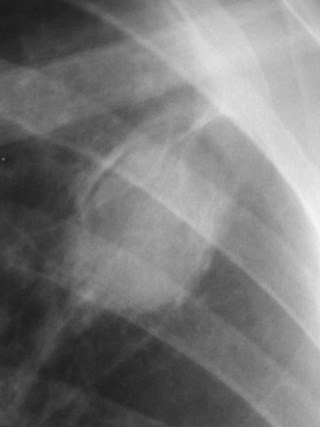
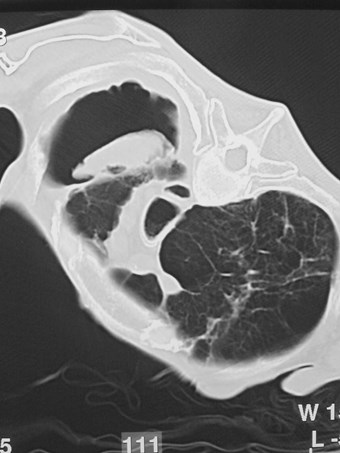
43 y.o. construction foremanfrom Puerto Rico



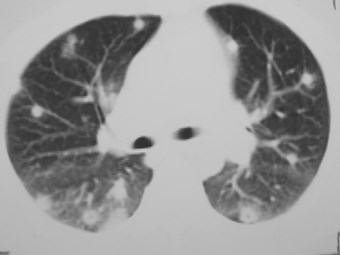
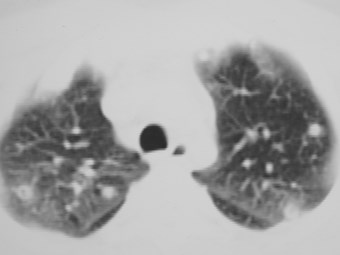
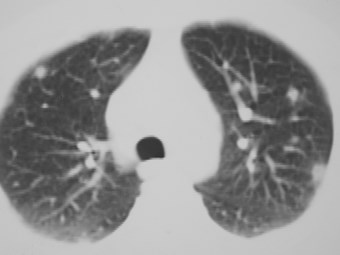


Several months later




Chronic Histoplasmosis
•Histoplasmoma
•Chronic progressivehistoplasmosis
•Mediastinal granuloma
•Fibrosing mediastinitis

Histoplasmoma
•Common, usually <3 cm.
•Central or ring calcification
•Calcified LN’s often also present
•Calcification does not always indicate“healing”
May grow over time, harbor viable organisms


“Target” lesion
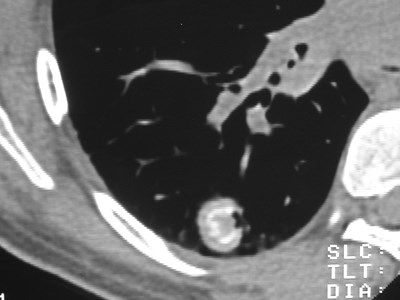
Laminar calcification

Chronic PulmonaryHistoplasmosis
•Almost always assoc. with emphysema
•Inflammation may be immune responseto antigens from colonizing organisms
•May progress to cavitation, fibrosis
•Radiographically indistinguishable frompostprimary TB, though may have lesssevere symptoms



Mediastinal Histoplasmosis
•MediastinalGranuloma
Conglomerateadenopathy
Often calcified
Usuallyasymptomatic

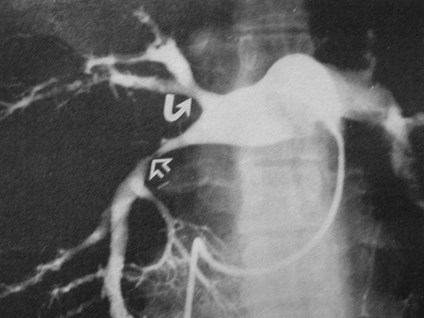
Mediastinal Histoplasmosis
•FibrosingMediastinitis
Leakage of antigen
Sclerosinginflammation whichmay calcify
Vascular, airway,esophagealinvolvement
Mimics cancer

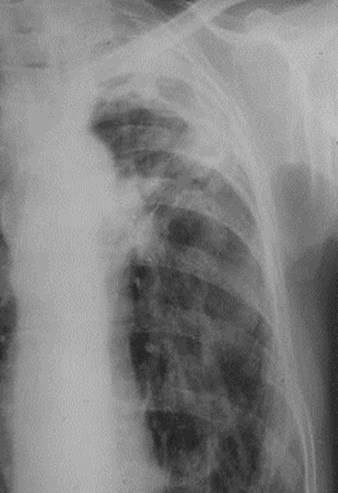
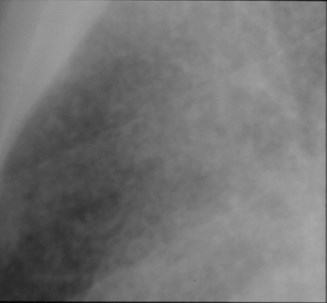
DisseminatedHistoplasmosis
•Opportunistic disease
1 in 2000 infections in immune competent
•Acute fulminant or subacute course
•Miliary pattern
•+/- diffuse linear opacities and irregularnodules
•Hepatosplenomegaly

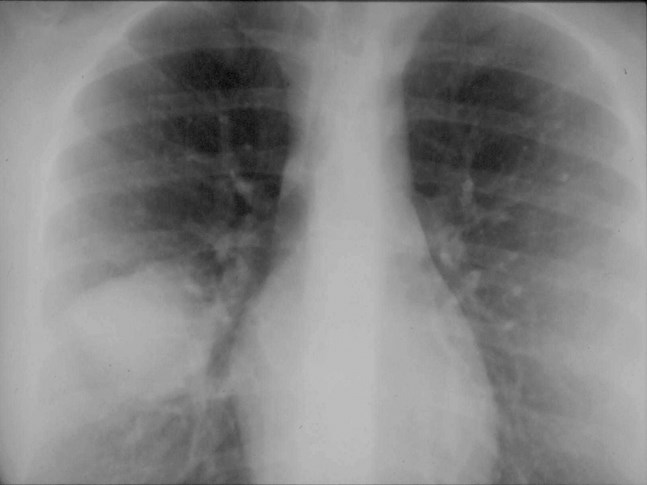
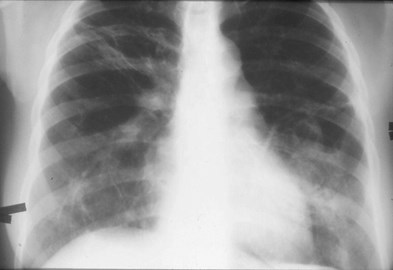
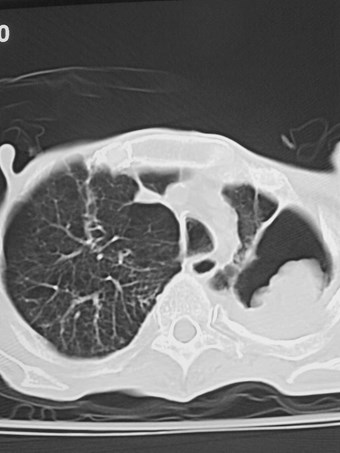
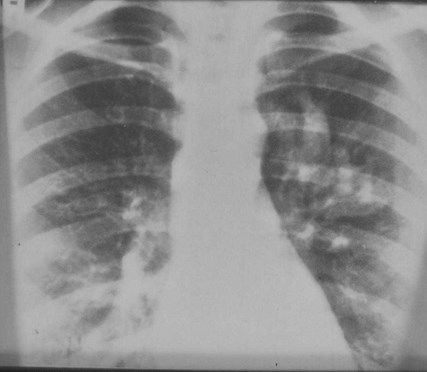
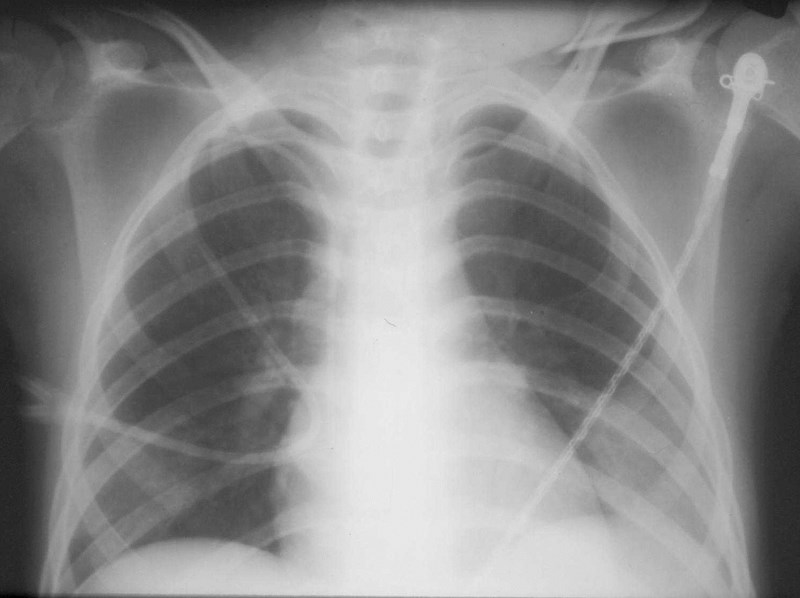
27 y.o. withAIDS, SOB

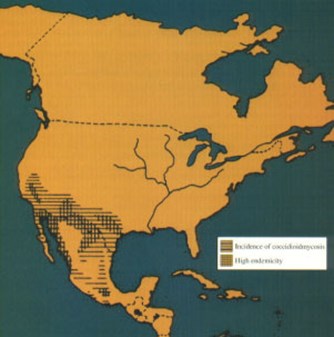
Coccidioidomycosis
•C. immitis: a soil saprophytein SW US
•Also endemic in many areasof South and CentralAmerica
•100,000 cases/yr in US
•Spores inhaled, change totissue-invasive hyphal form
•Cases seen in non-endemicareas due to travel toendemic area or reactivation

Coccidioidomycosis
•Acute “Valley fever”
•Persistent primary
•Chronic progressive
•Disseminated

CoccidioidomycosisClinical Features
•60% of cases asymptomatic
•15% mild sx
•5% disseminated infection
•“Valley fever”
2-3 week incubation period
Flu-like illness
Mild to severe respiratory disease
E. nodosum or E. multiforme
Resolves in 2-4 weeks

Acute CoccidioidomycosisRadiology
•Pneumonia with parenchymal consolidation (75%)
•Single or multiple foci
•May have acute transient cavities
•Streaky peribronchial densities
•Adenopathy in 25%, may be only finding
•Effusion in 20%, usually small

Persistent Primary Cocci
•Clinical or Xray findings after 6 weeksdefine persistent primary disease
<10 % of symptomatic cases
•Nodule (coccidioidoma)
•Cavitary disease
•Unusual progressive pneumonia

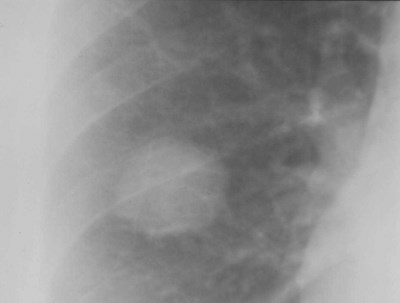
Coccidioidoma
•Almost always asymptomatic
•Develops from pneumonic process
•Usually <1.5 cm, single, peripheral,+/- cavitation
•Calcification uncommon
Differs from histo, TB

24 y.o. asymptomatic woman






Cavitary Cocci
•Cavities form fromnecrosis of nodules
Thin or thick wall (thin isclassic)
May fluctuate in size
Upper lobe, solitary
>50% asymptomatic, mayhave hemoptysis
50% resolve within 2 yrs

Chronic Progressive Cocci
•<1% of pulmonary cases
•Impaired host defenses
•Fibronodular or necrotizing withcavitation
•Resembles chronic TB, histo

Disseminated Cocci
•0.5% of white patients, 10-15% of non-whites (immune competent)
•Immune compromised patients
•Usually evident within weeks ofprimary infection
•Miliary disease in lungs
•Bones, joints, skin, meninges, LN’s
•Fatal in 50% if untreated

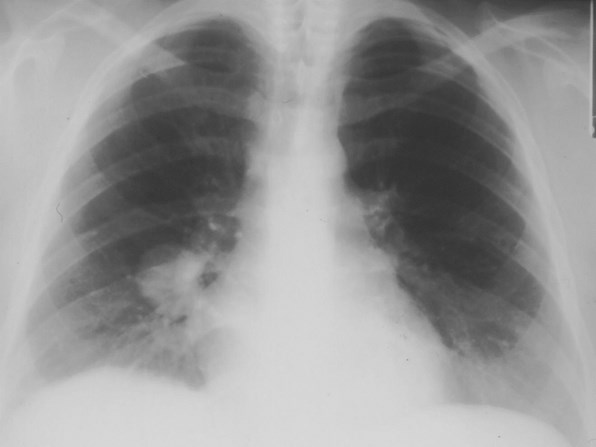
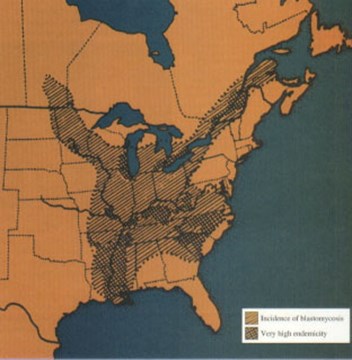
Blastomycosis
•Endemic areas broadly overlapw/ histo
•Much less common disease
•Serologic/antigen testsunreliable
•Acute clinical diseaseuncommon
•Chronic disease more common
Malaise, wt loss, CP, fever,mild cough
•Rare fulminant disease

Blastomycosis
•Highly variable appearance
Consolidation, often with air bronchogram
Focal mass
Interstitial disease
Miliary
•Commonly mimics bacterial pneumonia orbronchogenic Ca
Delay in diagnosis
Case fatality rate ~5%

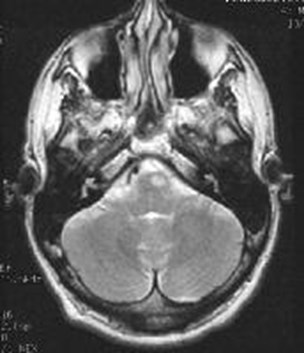
Blastomycosis
•Nodal enlargementuncommon
•Extrathoracic diseaserelatively common comparedto histo
Skin - characteristic lesions
Bone
Brain
Prostate




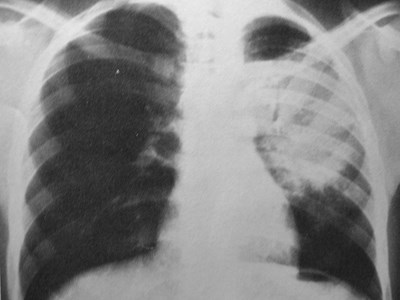
3 months later





Immunodeficient Host:Ubiquitous Fungi
•Cryptococcus neoformans
•Aspergillus fumigatus
•Candida sp. (esp. albicans)
•Zygomycetes
Mucor
Rhizopus
Absidia

Cryptococcosis
•C. neoformans a ubiquitous soilsaprophyte
•Pulmonary infection can occur in normalor compromised host
•Route of entry almost always inhalational
•Treatment only for progressive disease orcompromised host
Most pulmonary disease is asymptomatic

CryptococcosisCompetent Host
•Fungal “collections”
Rare
Growth in lung without inflammation
Often asymptomatic
Subpleural nodules or masses
•Nodules
most common form
Up to several cm in size
Ca++ rare

CryptococcosisCompetent host
•Pneumonia
Acute form rare, sx usually subacute
May be bilateral
Adenopathy common
•Disseminated
Rare in normal host
Common in compromised host

CryptococcosisCompromised Host
•Most common fungal pathogen in AIDS
•Second most common in transplantpatients after Aspergillus
•Pneumonic consolidation or diffuse
Mimics PCP
•Cavitation (<25%)
•Adenopathy
•CNS disease coexists commonly in AIDS
•Disseminated disease common in AIDS


40 y.o. S/P renal txp




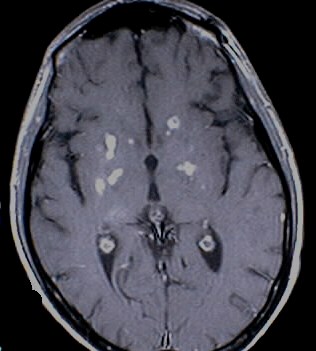


27 y.o. with AIDS



Aspergillosis
•Aspergillus fumigatus -- ubiquitoussaprophyte
•Unusual cause of disease in normal host
•Spores inhaled, ingested bymacrophages
•Spores can convert to invasive hyphalform

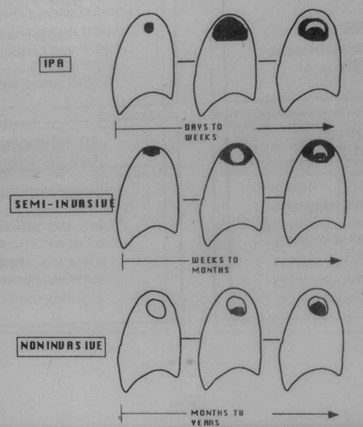
AspergillosisForms of Disease
•Depend on host immune state
Normal - mycetoma
Mild compromise - semi-invasive
Compromised - IPA
Hyperimmune – ABPA
Immune status
hyperimmune
compromised
competent
ABPA
mycetoma
semi-invasive
IPA

Mycetoma(“Fungus Ball”, Aspergilloma)
•Non-invasive form - saprophytic growth ina pre-existing cavity (TB, sarcoid, bulla)
•Cavity is “sheltered” from the immunesystem
•Vascular granulation tissue lines cavity
•Pleural reaction locally

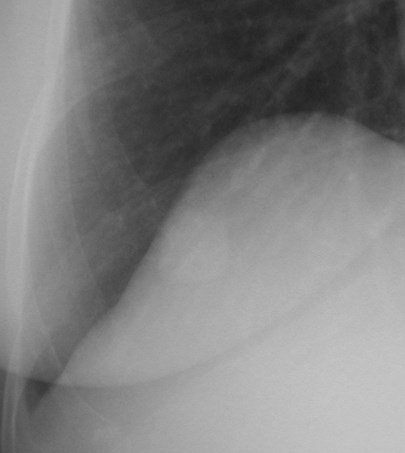
Mycetoma
•CXR/CT: Hallmark is a mobile mass withina cavity
•Decubitus or prone views
•May have severe hemoptysis
•Systemic antifungals ineffective
•Rx: resection, embolization, intracavitaryantifungal(?)




Semi-invasive Aspergillosis“chronic necrotizing Aspergillosis”
•Underlying host disease
DM, sarcoid, debilitation, COPD, ETOH
•Indolent necrotizing granulomatousinfection
•Constitutional sx, chronic cough,fever, sputum

Semi-invasive Aspergillosis
•Upper lobes
•+/- mycetoma
•Treatment only for sx

Invasive PulmonaryAspergillosis (IPA)
•Primary form (normal host) rare
•Secondary form - severelyimmunocompromised patients
Acute leukemia on chemotherapy
AIDS
Corticosteroid use
Cytotoxics
Organ transplant

Invasive PulmonaryAspergillosis
•Organism invades tissue, thrombosesarteries infarction of lung tissue
•Sx: Fever cough, pleuritis, dyspnea
•Dx: TBBx (+) only in 50%, often need OLBx
•Rx: IV Ampho-B
•Mortality 90% in transplant pts, 35% inleukemia pts

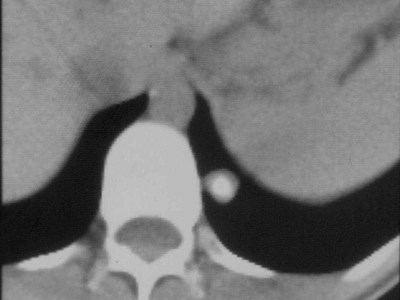
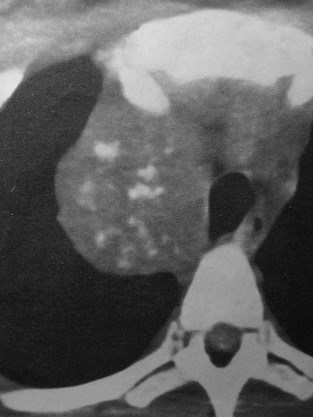
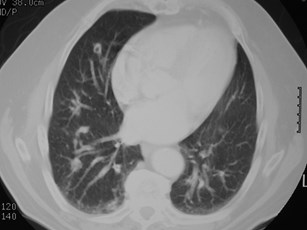
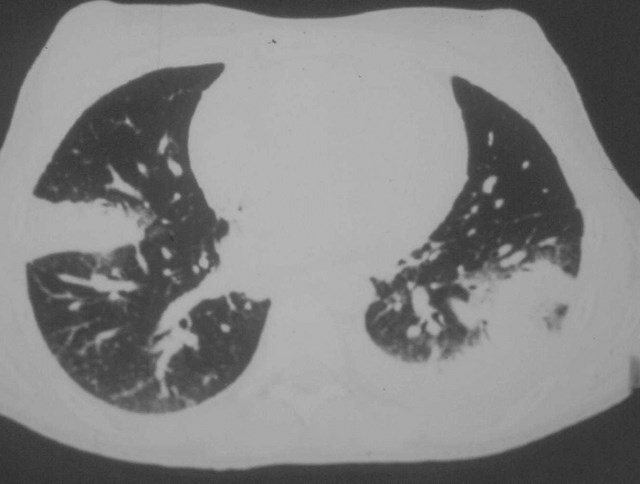
Invasive PulmonaryAspergillosis
•Rapidly progressive pneumonia
•Multifocal or localized
•Often nodular early, progresses toconfluence
•“Air crescent” sign late as immunesystem recovers and cavitation occurs
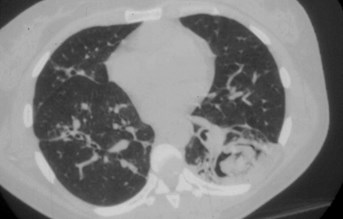
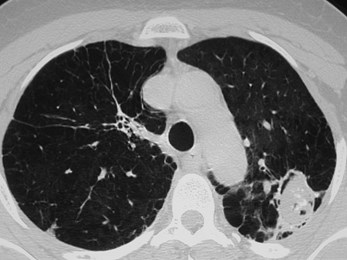
•CT “halo” sign


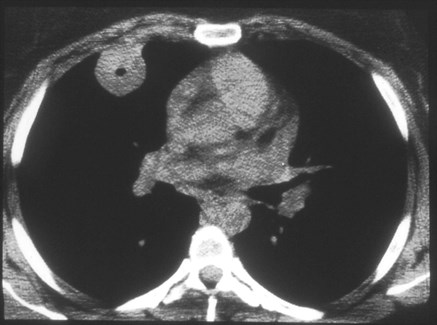
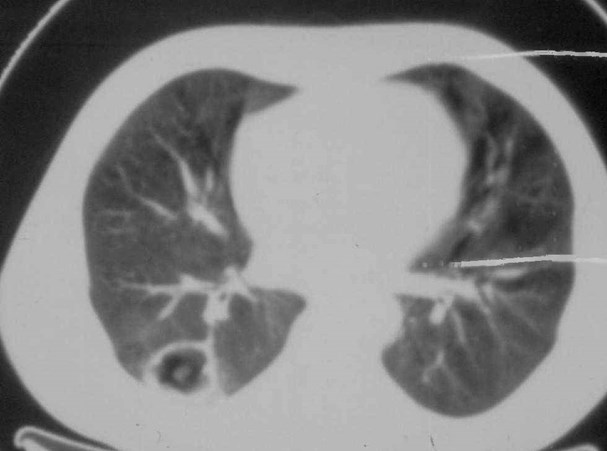
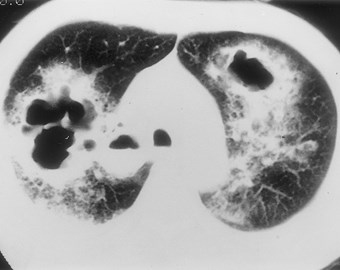
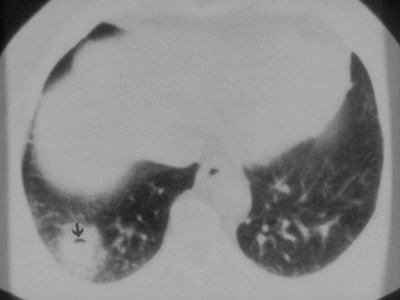
67 y.o. with leukemia
3 days later

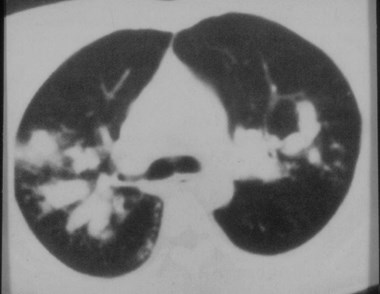
CT “halo” sign

Aspergillus Infectioncharacteristic appearances

Allergic BronchopulmonaryAspergillosis (ABPA)
•Asthmatics
•Noninvasive endobronchial fungal growth
•Antigens stimulate hypersensitivity reaction
•Excess mucus containing organisms andeosinophils
•Inflammation leads to bronchiectasis
•Clinical :
Fever, pleuritis, eosinophilia, expectoration of plugs
Occasionally aymptomatic

ABPA
•CXR: central bronchiectasis with mucoidimpaction
•“rabbit ears”, “fingers in glove”
•Occ. Atx, fibrosis, migratory opacities
•Rx: Steroids


BronchocentricGranulomatosis
•Rare disease-final pathway of several insults?
•Necrotizing granulomas centered on bronchi
•Aspergillus found inside granulomas in40-50% of asthmatics. Not found innonasthmatics with BG.
•Same pathology seen in other infections:
TB, endemic fungi
•Eosinophilia in blood
•Usually radiographic appearance of ABPA
•Nodule(s) or consolidation can mimic Ca

Candidiasis

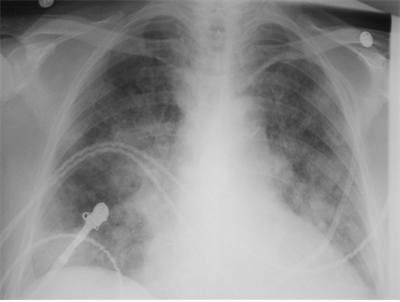
15 y.o. diabeticwith fever

Mucormycosis

Final page of the radiology boards


Pulmonary Fungal DiseasesTake-Home Messages
•Remember endemic areas!
•Histo: Nodules, chronic fibroproductivedisease mimics TB
•Cocci: Nodules or thin-walled cavities
•Blasto: Mass-like lesions
•Crypto: AIDS patients, nodules, cavitation
•Aspergillus: Mycetoma, fulminant invasiveform, ABPA

Thank you